Blood Cancers
Overview
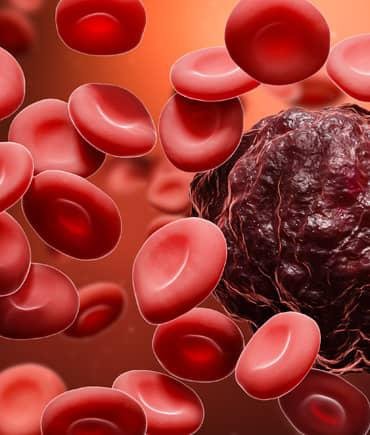
Blood cancer endangers an essential life force — our blood cells. These cells give us energy, help us fight infection and keep us from bleeding too much. Blood cancer affects how your body produces blood cells and how well those cells work. Fortunately, there are many effective and safe ways to treat blood cancer.
What is blood cancer?
Blood cancer affects how your body produces blood cells and how well those cells work. Most blood cancers start in your bone marrow, the soft, sponge-like material in the center of your bones. Your bone marrow makes stem cells that mature and become red blood cells, white blood cells and platelets.
Normal blood cells fight infection, carry oxygen throughout your body and control bleeding. Blood cancer happens when something disrupts how your body makes blood cells. If you have blood cancer, abnormal blood cells overwhelm normal blood cells, creating a ripple effect of medical conditions. More people are living longer with blood cancer, as healthcare providers find new ways to treat it.
Are blood cancers serious?
Blood cancers are serious illnesses, but other cancer types are more deadly. Blood cancers represent about 10% of all cancers diagnosed and an estimated 3% of all cancer-related deaths. National Cancer Institute data show a steady decline in blood cancer deaths.
Types of blood cancer?
There are three blood cancer types, each with several subtypes. Those cancer types and subtypes are:
- Leukemiais the most common blood cancer in the United States and the most common cancer among children and teenagers. The five-year survival rate has quadrupled over the past 40 years. Types of leukemia include , acute meyeloid leukemia, chronic lymphocytic leukemia, chronic meylogenous leukemia and acute lymphoblastic leukemia.
- Lymphomais cancer of your lymphatic system, which includes your bone marrow. The survival rate has doubled over the past 40 years. Types of lymphoma include Hodgkin lymphoma, non- Hodgkin lymphoma, Waldenstrom macroglobulinemia, follicular lymphoma, B-cell lymphoma and Cutaneous T-cell lymphoma.
- Myeloma is cancer that starts in your bone marrow and affects your plasma cells. Multiple myeloma is the most common myeloma type. More than half of people diagnosed with myeloma are alive five years after diagnosis. Other types of myeloma include plasmavytoma and amyloidis.
What causes blood cancer?
Researchers know blood cancer happens when blood cell DNA changes or mutates, but they aren’t sure why this happens. Your DNA tells cells what to do. In blood cancer, DNA tells blood cells when to grow, when to divide or multiply and/or when to die.
When DNA gives your cells new instructions, your body develops abnormal blood cells that grow and multiply faster than normal and sometimes live longer than normal. When that happens, normal blood cells become lost in an ever-growing horde of abnormal cells that crowd your normal cells and monopolize space in your bone marrow.
Eventually, your bone marrow produces fewer normal cells. That means there aren’t enough normal cells available to do their essential tasks: carrying oxygen through your body, fighting infection and controlling bleeding. Here’s how genetic change may cause the three blood cancer types:
- Leukemia: Researchers think leukemia happens when a combination of environmental and genetic factors triggers DNA changes. In this case, researchers think changes in chromosomes may trigger DNA changes. Chromosomes are strands of DNA. When cells divide and make two new cells, they copy these DNA strands. Sometimes, genes from one chromosome switch to another chromosome. In leukemia, this switch may affect a set of genes that help cells grow and another set of genes that suppress tumors. Researchers believe exposure to high levels of radiation or certain chemicals plays a role in the genetic changes that cause leukemia.
- Lymphoma: Lymphoma happens when there’s a change in genes in white blood cells, called lymphocytes, that causes them to multiply uncontrollably. In addition, abnormal lymphocytes don’t die when normal lymphocytes die. Again, researchers don’t know what triggers the genetic change, but research shows certain infections or having a depressed immune system may be factors.
- Myeloma: In this case, plasma cells in your bone marrow get new genetic instructions that make them multiply. Researchers are investigating potential links between myeloma and chromosomal change that affect genes that control plasma cell growth.
Symptoms of blood cancer
Blood cancer symptoms vary based on blood cancer type, but there some symptoms all three have in common:
- Fatigue: This is feeling so tired you can’t manage your daily activities. You may also feel weak.
- Persistent fever: A fever is a sign your body is fighting infection or responding to abnormal cancer cells.
- Drenching night sweats: This is sweating that comes on suddenly while you’re sleeping, disturbing your sleep and drenching your bedding and clothes.
- Unusual bleeding or bruising: Everyone has bumps, bruises and injuries that make us bleed. Unusual bleeding or bruising is bleeding that doesn’t stop and bruises that don’t heal after two weeks.
- Unexpected or unexplained weight loss: Unexpected weight loss of 10 pounds over a six- to 12-month period is considered unexplained weight loss.
- Frequent infections: Frequent infections may be a sign something is affecting your immune system.
- Swollen lymph nodes or an enlarged liver or spleen: These symptoms may be signs of leukemia or lymphoma.
- Bone pain: Myeloma and leukemia may cause bone pain or tender spots on your bones.
Many blood cancer symptoms are similar to other less serious illnesses’ symptoms. Having any of these symptoms doesn’t mean you have blood cancer. But you should contact your healthcare provider when you notice symptoms or changes in your body that last more than a few weeks.
Diagnose blood cancer
Healthcare providers may begin diagnosis by asking about your symptoms and your medical history. They’ll do complete physical examinations. They may order several kinds of blood and imaging tests, too. The tests they’ll use may be different for each suspected blood cancer type. Tests used to diagnose blood cancer include:
- Complete blood count (CBC):This test measures and counts your blood cells. For example, if your healthcare provider suspects you have leukemia, they’ll look for high (or low) white blood cell counts and lower than normal red blood cell and platelet counts.
- Blood chemistry test: This test measures chemicals and other substances in your blood. In some cases, your healthcare provider may order specific blood test for cancer to learn more about your situation.
- Comutarised tomography (CT) scan: : This test uses a series of X-rays and a computer to create three-dimensional images of your soft tissues and bones. If your healthcare provider suspects you have myeloma, they may order a CT scan to look for bone damage.
- Magnetic resonance imaging (MRI) scan: Your healthcare provider may order an MRI to look for signs of leukemia or lymphoma complications affecting your spine.
- Positron emission tomography (PET) scan: This test produces images of your organs and tissues at work. Your healthcare provider may order a PET scan to look for signs of myeloma.
- Bone marrow biopsies: Healthcare providers may do bone marrow biopsies to analyze the percentage of normal and abnormal blood cells in your bone marrow. They may also test your bone marrow sample for changes in your DNA that may drive cancer growth.
- Blood cell examination: Healthcare providers may take blood samples so they can examine them under a microscope to look for changes in blood cell appearance. For example, they might order peripheral smear test to look for signs of leukemia or lymphoma.
Treatment of blood cancers
Blood cancer treatment isn’t one-size-fits-all. Some blood cancer types respond well to specific treatments. Some blood cancer treatments have significant side effects. Healthcare providers consider factors, including your age, your overall health, the kind of blood cancer you have and specific treatment side effects, before recommending a treatment plan. Some common treatments for blood cancer include:
- Chemotherapy: Chemotherapy is a primary blood cancer treatment, killing cancer cells to either slow down the disease’s progress or eliminate the cancer. Healthcare providers use different drug types for different blood cancers.
- Radiation therapy: Healthcare providers may use radiation to treat leukemia, lymphoma or myeloma. Radiation targets abnormal cells, damaging their DNA so they can’t reproduce. Healthcare providers often combine radiation therapy with other treatments. They may use radiation to ease some symptoms.
- Immunotherapy: This treatment uses your immune system to fight cancer. Immunotherapy may help your body make more immune cells or help your existing immune cells find and kill cancer cells.
- Targeted therpy:This cancer treatment targets genetic changes or mutations that turn healthy cells into abnormal cells.
- CAR T-cell therapy: In CAR T-cell therapy, healthcare providers turn T-cell lymphocytes — a type of white blood cell — into more effective cancer treatment. Healthcare providers may use CAR T-cell therapy to treat B-cell acute lymphoblastic leukemia, multiple myeloma and several types of non-Hodgkin’s lymphoma if other treatments haven’t worked.
- Atologous stem cell transplsnt: Healthcare providers can collect and store bone marrow stem cells before administering high doses of chemotherapy. Once chemotherapy is done, they’ll replace the protected stem cells. This way, people having autologous stem cell implants can avoid chemotherapy side effects.
- Allogeneic stem cell transplsnt: Sometimes, damaged bone marrow needs to be replaced with healthy bone marrow. Healthcare providers identify a suitable bone marrow donor and use the donor’s cells to replace your damaged ones. This is an effective but dangerous procedure.
How can I reduce risk for developing blood cancer?
Blood cancer happens when blood cell DNA changes or mutates. Researchers don’t know why this happens, which makes it hard to single out specific steps someone could take to reduce their risk. But researchers have identified some factors that appear to play to a role in the genetic change:
- Radiation exposure.
- Certain chemicals.
- Lowered immunity due to infections.
- Family history of blood cancer.
- Inherited conditions that increase the risk of developing blood cancer.
Can blood cancer be cured?
Yes. Often, the goal of blood cancer treatment is curing the condition. But when a cure isn’t possible, there are a growing number of treatments that may put some blood cancers into remission. Remission means the treatment eliminates cancer signs and symptoms for a long time.

